zoloft for sex
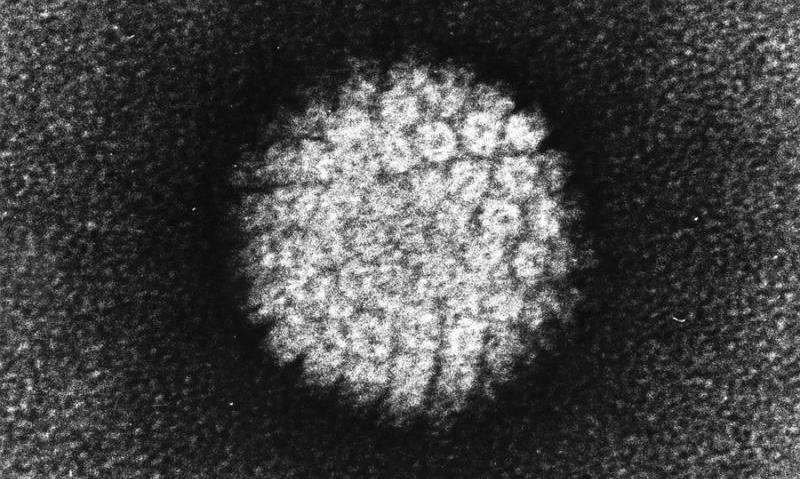
Vaccinating adults age 26 and older against the human papillomavirus (HPV)—the virus that causes more than 90% of cervical cancers as well as several other cancers—may not be cost-effective, according to a new study led by researchers at the Harvard T.H. School of Public Health.
“Our study found that the added health benefit of increasing the vaccination age limit beyond 26 years is minimal, and that the cost-effectiveness is much lower than in pre-adolescents, the target age group for the HPV vaccine,” said Jane Kim, buy cephalexin uk no prescription K.T. Li Professor of Health Economics and lead author of the study.
The study will be published March 11, 2021, in PLOS Medicine.
HPV vaccines have been shown to be highly effective in preventing HPV infections that are associated with cervical, anal, oropharyngeal, vulvar, vaginal, and penile cancers, as well as genital warts. Current U.S. guidelines recommend HPV vaccination for girls and boys at age 11 or 12, and catch-up vaccination for people through age 26 if they were not vaccinated when younger. For adults beyond age 26, the guidelines don’t specifically recommend catch-up vaccination but suggest that, for people aged 27-45, clinicians and patients make decisions about HPV vaccination on an individual basis.
The new study, undertaken to inform these national guidelines, used two mathematical models—from Harvard and Cancer Council New South Wales, Australia—that simulated scenarios of extending HPV vaccination to women and men up to age 45 years. Using U.S. data, the models projected cost and health outcomes of the six HPV-associated cancers and genital warts, taking into account historical and future vaccination uptake in younger people, cervical cancer screening practices among women, vaccine efficacy, and vaccination costs. The researchers sought to determine whether the benefits of HPV vaccination at older ages would have an incremental cost-effectiveness ratio (ICER) that was in line with a commonly-cited upper threshold of $200,000 per quality-adjusted life year (QALY). QALYs are a measure of life expectancy adjusted to account for quality of life associated with health conditions and events.
The researchers found that HPV vaccination beyond age 26 in the U.S. would provide limited health benefit at the population level, at a substantial cost, given current HPV vaccine prices. Their analysis showed that the ICER for vaccinating people up to age 45 years ranged from $315,700 to $440,600 per QALY gained.
Kim noted that current HPV vaccines are prophylactic and therefore most effective when given prior to HPV exposure, which can happen soon after sexual initiation; once someone is exposed to HPV, the vaccine won’t clear those infections. “By the time you vaccinate individuals in their 30s and 40s, many have already been exposed to HPV, so the health benefit really decreases at these older ages,” she said. “It’s also important to emphasize that cervical cancer screening remains an effective and cost-effective way to protect women from cervical cancer.”
Source: Read Full Article
