Barrett's Esophagus Preventing Progression
By Jeyashree Sundaram (MBA)
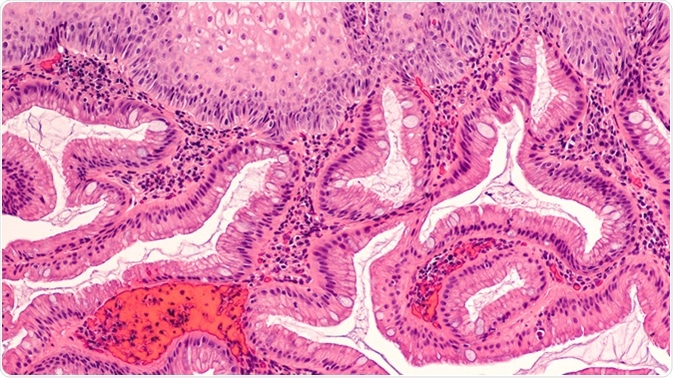
Barrett's Esophagus, which is a condition in which tissues that resembles the tissues of the intestinal lining, substitutes the tissues that line the esophagus. This is not a malignant disease unless the abnormal chances in the tissue progresses to dysplasia and then esophageal cancer.
Preventing the progression of this condition to high-grade dysplasia and cancer is very vital in order to reduce the possible complications as well as improve the survival chance of the patients.
Treatments to minimize the risk of cell transformation into malignancy are available to patients affected by BE and this can greatly help them from becoming dysplastic.
Preventing Progression of Barrett's Esophagus to Cancer
There are myths that state that there is no treatment available to cure Barrett's esophagus. Although clinically the basic treatment for BE without dysplasia is done by controlling the exposure of the esophageal acid with the help of proton pump inhibitor (PPI) medicines such as omeprazole (Prilosec), usually this controlling process is done once or twice a day, depending upon the need.
Studies also report that the cancer risk for people with BE is lesser in patients who consume aspirin or other anti-inflammatory drugs (for e.g., ibuprofen). However, regular intake of these drugs may result in bleeding in the stomach and damage to the kidney. Another drug called statins also helps in minimizing the risk of cancer; these are used to control high cholesterol level.
The first line treatment for this condition is surgical procedure to permanently stop the acid reflux action, which is called anti-reflux surgery. But the sad truth is that, restraining this acid reflux may not prevent Barrett's tissue from transforming into cancer.
- If the healthcare provider identifies dysplasia in any biopsies, the method of treatment changes depending on the grades of dysplasia. Dysplasia falls under two categories: low-grade dysplasia and high-grade dysplasia.
- If the patient is identified with low-grade dysplasia, the physician recommends a tight surveillance with every six to twelve months of ablation or endoscopy.
- If the patient is found with high-grade dysplasia, endoscopic therapies are performed to eradicate the Barrett's tissues.
- In the case of early cancer, endoscopic procedure is carried out to destroy the cancer present in the specific part of the cell, and this is followed by surgery or destruction of tissue.
In one study it was showcased that, as long as the acid reflux is repressed, there will be a regrowth of squamous tissue in the area of destructed Barrett's tissue.
Tissue Destruction Using Endoscopy
Endoscopic tissue destruction can be performed using various methods:
- Photo dynamic therapy (PDT): This therapy is an aggressive technique that is a combination of laser treatment and photo-sensitizing medication, and is effective enough to destroy the cancerous tissue. The side effects comprise light sensitivity (avoidance of natural light for a month) and pain or stricturing in the esophagus. This therapy is not very commonly used.
- Endoscopic mucosal resection (EMR): This technique involves vaccinating saline into the lining of the esophagus and shaving off the small-sized tissues that are overlapped to remove vast areas requiring resection. EMR eradicates the tissues and paves the way for the pathologist to investigate bigger pieces for the existence of cancer in the smaller areas that have not been identified.
- Radiofrequency ablation (RFA): In this process a balloon is wrapped with slim electric coils that can provide a minor burst of composed heat. This heat is capable of destroying the outer most layer of the tissue without disturbing the inner structures of the tissue. This technique is widely used to treat Barrett's esophagus.
- Cryoablation: The process of cryoablation is performed by spraying liquid nitrogen with the help of an endoscope; this method is capable to freeze the Barrett's tissue.
- Argon plasma coagulation: This technique is described as a “touch up treatment” targeted at the areas where the Barrett's tissue might have survived. In this method, bleeding lesions are coagulated by ionized jet of argon plasma through endoscopy ignition of electric pulse.
Even years after the success of ablation therapy, there are chances for the development of cancer in the esophagus. It is advisable to make close follow-ups by participating in biopsy or endoscopy at one- to two-year intervals. Having regular follow-ups even there is no Barrett's esophagus leftover after treatment would be a wise call.
It has been reported that centers performing treatments for greater volumes of Barrett's esophagus and dysplasia patients have attained vast success by making patients avoid progression or surgery of their cancers.
Experienced centers coordinate care tightly with physicians, gastroenterologists, and care crew members to make sure of follow-ups to control symptoms and to monitor side effects.
It is advisable for these patients to be in contact with expert surgeons who can help them with the knowledge of options for both anti-reflux and definitive surgery in the case when medications do not produce effective results.
Sources
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2387291/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3016471/
- prevention.cancer.gov/funding-and-grants/funded-grants/P01CA091955
- http://www.gastro.org/guidelines/barrett-s-esophagus-1
- http://www.aafp.org/afp/2014/0115/p92.html
Further Reading
- All Barrett's Esophagus Content
- Barrett’s Esophagus – What is Barrett’s Esophagus?
- What Causes Barrett’s Esophagus?
- Barrett’s Esophagus Symptoms
- Barrett’s Esophagus Pathology
Last Updated: Aug 23, 2018
Source: Read Full Article
