COVID-19 and Opioids
Opioids are drugs that interact with opioid receptors mainly located in the brain and central nervous system, usually medically administered as pain relief or anesthesia. Morphine is perhaps the most widely used and well-known opioid in a medical setting, while the very similarly structured sister chemical heroin is well known as an illicit substance with few medical uses, though is still used in some palliative care instances.
Opioids have been shown to affect the ordinary functioning of the immune system, and this may have significant implications for COVID-19 patients.
 Image Credit: Iryna Imago / Shutterstock.com
Image Credit: Iryna Imago / Shutterstock.com
There are several types of opioid receptors, and an opioid may interact with only one type or multiple in either an agonistic or antagonistic way, with a range of affinities. These receptors play important endogenous roles in body homeostasis.
For example, endorphins are naturally produced in the pituitary gland and interact with one type of opioid receptor to produce analgesic effects, lowering the heart and breathing rate. Conversely, another endogenously produced biomolecule named enkephalin interacts with the same receptor to produce no analgesic effects, though is involved in cardiovascular modulation.
Opioids and the immune system
Opioids are capable of modulating the immune system, suppressing or enhancing the proliferation of B and T lymphocytes, causing these and other cells to undergo apoptosis, or diminishing leukocyte activity, depending on the specific drug. Some opioids, including morphine, have been noted to suppress the cellular immune system against bacterial infection, while others such as codeine have not been found to have any effect.
Morphine causes a reduction in the number of macrophages and T cells expressed in animal models, though the precise reason behind this effect is yet to be determined. Opiate users are well reported to suffer more greatly and frequently from serious bacterial infections, and past reports indicate the incidence of pneumonia among these groups is around ten times higher than average.
T and B lymphocytes express opioid receptors on their surface, and so their activity is modulated by interaction with opioids. One study demonstrates that patients administered morphine for pain relief over a period of 12 months express the complementary receptor more greatly on the surface of T and B lymphocytes, reinforcing the magnitude of effect.
Some opioids interacting with T lymphocytes have been shown to induce the release of interleukin-4, a cytokine with anti-inflammatory effects, while those interacting specifically with morphine downregulate the release of this molecule.
Monocytes and macrophages, the first line of defense against pathogens, are also affected by opioids. Animal studies have demonstrated that morphine significantly delays the entry of immune cells into the lung tissue in pneumonia-affected subjects, though such effects appear to be dose dependant, with lower concentrations in fact enhancing the ability of mice to fight Leishmania infection.
Although each mechanism underlying the way in which opioids modulate the immune system is not yet completely clear, the evidence of modulation is apparent but diverse. Some opioids may have a positive, negative, or neutral effect on various aspects of immune function that are dose and chronicity-dependent.
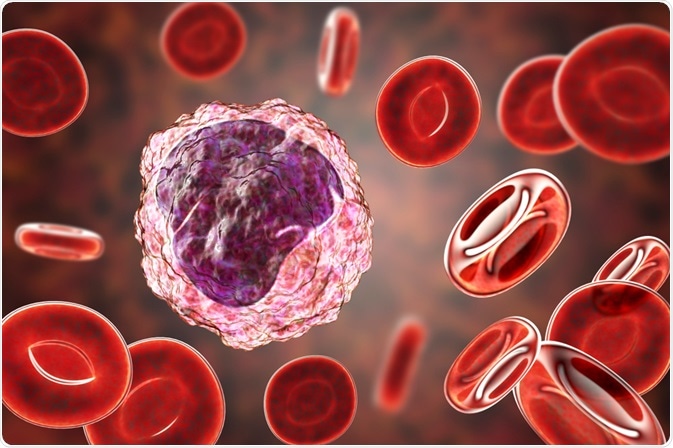 Monocytes and macrophages, the first line of defense against pathogens, are also affected by opioids. Image Credit: Kateryna Kon / Shutterstock.com
Monocytes and macrophages, the first line of defense against pathogens, are also affected by opioids. Image Credit: Kateryna Kon / Shutterstock.com
How could opioids affect COVID-19 prognosis?
Immune suppression caused by the use of opioids could facilitate the initial infection with SARS-CoV-2. Many patients suffering from severe SARS-CoV-2 infection experience inflammatory cascades and a cytokine storm, the excessive reaction of the immune system that contributes heavily towards mortality, at late stages of disease progression.
A suppressed immune system, therefore, could in fact play a protective role against extreme immune response. Indeed, in the course of initial SARS-CoV-2 infection anti-viral agents that help to reduce proliferation have been shown to be very effective, while once late-stage severe symptoms induced by the cytokine storm begin to appear immunosuppressive drugs are employed and have shown success. Therefore, immune suppression is at first disadvantageous and then could potentially become advantageous at later stages.
As discussed, the effect of opioids on the immune system is highly dependent on the specific drug, the size of the dose applied, and the chronicity of use. Chronic users are likely to bear numerous comorbidities that influence the course of disease progression, and it must be noted that the additional physical and psychological stresses induced by social isolation and lessened access to services throughout the pandemic could further encourage users to relapse or overdose. The CDC states that recorded deaths from overdoses have spiked by nearly 40% in the 12 month period of summer 2019 to 2020 compared with the previous year.
An analysis of US electronic health records undertaken by Wang et al. (2020) found that those recently diagnosed with substance abuse disorder (any drug, including opioids) were around eight times more likely to contract COVID-19, while opioid users specifically were ten times more likely. Hospitalization and death rates among those with substance abuse disorder were 10% and 3% higher than the average for all COVID-19 patients, respectively.
References
- Wang, J., Barke, R. A., Ma, J., Charboneau, R. & Roy, S. (2008) Opiate abuse, innate immunity, and bacterial infectious diseases. Archivum Immunologiae et Therapiae Experimentalis, 56. https://link.springer.com/article/10.1007%2Fs00005-008-0035-0
- Liang, X., Liu, R., Chen, C., Ji, F. & Li, T. (2016) Opioid System Modulates the Immune Function: A Review. Translational Perioperative and Pain Medicine, 1(1). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4790459/
- Steffens, C., Sung, M., Bastian, L. A., Edelman, E. J., Brackett, A. & Gunderson, C. G. (2020) The Association Between Prescribed Opioid Receipt and Community-Acquired Pneumonia in Adults: a Systematic Review and Meta-analysis. Journal of General Internal Medicine, 35(11). https://pubmed.ncbi.nlm.nih.gov/32885375/
- Wang, Q. Q., Kaelber, D. C., Xu, R. & Volkow, N. D. (2020) COVID-19 risk and outcomes in patients with substance use disorders: analyses from electronic health records in the United States. Molecular Psychiatry, 26. https://www.nature.com/articles/s41380-020-00880-7
- Ataei, M., Shirazi, F. M., Lamarine, R. J., Nakhaee, S. & Mehrpour, O. (2020) A double-edged sword of using opioids and COVID-19: a toxicological view. Substance Abuse Treatment, Prevention, and Policy, 15. https://substanceabusepolicy.biomedcentral.com/articles/10.1186/s13011-020-00333-y#:~:text=The%20opioids%20modulation%20of%20the,of%20this%20class%20of%20agents.
- CDC (2020) Overdose Deaths Accelerating During COVID-19 https://www.cdc.gov/media/releases/2020/p1218-overdose-deaths-covid-19.html
Further Reading
- All Coronavirus Disease COVID-19 Content
- What Mutations of SARS-CoV-2 are Causing Concern?
- Long-term Effects of COVID-19 in Athletes
- What is the Clinical Impact of COVID-19 on Cancer Patients?
- Can Pets Get COVID-19?
Last Updated: Feb 12, 2021

Written by
Michael Greenwood
Michael graduated from Manchester Metropolitan University with a B.Sc. in Chemistry in 2014, where he majored in organic, inorganic, physical and analytical chemistry. He is currently completing a Ph.D. on the design and production of gold nanoparticles able to act as multimodal anticancer agents, being both drug delivery platforms and radiation dose enhancers.
Source: Read Full Article
