Cysts and scarring
Acne is an inflammatory disorder of the pilosebaceous units of the skin. These consist of the hair follicle, a fine canal leading off the skin surface, which is lined by keratinocytes giving rise to the hair shaft. Laterally attached to the hair follicle is the sebaceous gland, an oil-producing gland. The sebum is the secretion of these glands, and carries cellular debris including dead keratinocytes to the surface of the skin.
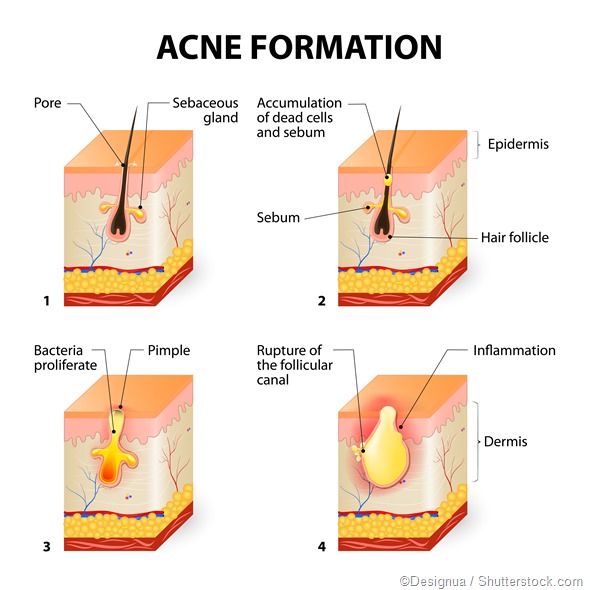
Acne results from the comedo, the lesion which is characteristic of this condition. The comedo is a blocked and enlarged hair follicle which is plugged up, leading to the accumulation of sebum and other follicular debris. Four factors give rise to acne:
- Sebaceous gland overgrowth leading to excessive production of sebum.
- Increased keratin production – this results in abnormal shedding of the keratinocytes in the hair follicle, which causes the canal to become obstructed forming a microcomedo (which is not visible to the eye).
- Inflammatory mediators such as cytokines and lipids which accumulate along with the sebum.
- Increased growth of Propionibacterium acnes, a normal skin commensal bacterium, which produces chemicals that further aggravate inflammation within the blocked follicle.
After this condition persists for some time, the weakened follicular wall may rupture, releasing these chemical mediators and bacteria into the surrounding skin to produce a larger area of infection and inflammation, resulting in nodular or cystic acne. The lesions are larger, deeper, and less firm, and usually leave scars if they are picked.

Diagnosis
Acne lesions are most common on the face, neck, upper arms, chest, and upper back. They may consist of the typical white (whiteheads) or blackish dots (blackheads) which evolve from the microcomedo as sebum accumulates and enlarges the follicle. More severe forms include the papular and pustular forms, which represent the onset of frank inflammation and infection, respectively.
The nodulocystic form is the most severe form, consisting of large firm or fluctuant masses deep within the skin, without a point for the contained pus. These are more than 0.5cm in diameter. These usually heal by scarring with hyperpigmentation. When more than a few nodulocystic lesions are present, the patient is treated for severe acne.
Treatment
Self-help for acne consists of washing the face with mild non-irritant soaps, twice a day, and keeping the skin free of excessive oil. If the hair is oily, it should be washed every day or on alternate days. Moisturizers and makeup used, if any, should be non-comedogenic.
Medical treatment of nodulocystic acne consists of:
1. Systemic tetracyclines
Examples include: doxycycline or minocycline, or macrolide antibiotics such as erythromycin. These have side effects ranging from the emergence of drug resistance with macrolides to teratogenic effects such as slowing of skeletal growth and tooth discoloration, and photosensitivity in response to the tetracyclines. They may take 6-8 weeks to show significant improvement in the acne, and must be continued for 6 months. More long-term treatment may be required for patients with severe cystic acne to prevent scarring.
2. Oral contraceptives
That contain progestins with low androgenic effects are used to contain acne.
3. Isotretinoin
A systemic vitamin A analog which is used for severe nodulocystic acne, because it inhibits all four factors that contribute to the development of this condition. It may be severely teratogenic and is therefore available only under the SMART (System for Management of Accutane-Related Teratogenicity) system to track and minimize its effects on developing fetuses. This system aims to avoid its use in pregnancy and minimizing the rate of conception when on this drug as far as possible.
4. Intralesional injection of corticosteroids
When acne fails to respond to this management, intralesional injection of corticosteroids may be needed. Other syndromes should be ruled out such as the association with hidradenitis suppurativa and dissecting scalp cellulitis.
Acne scars
Scarring is one of the most distressing sequelae of acne, affecting up to 1 in 10 people with acne. How the scars are treated depends on their depth and location, as well as the type of scar. Scars are classified as:
1. Atrophic scars
These are the most common and are subdivided into:
- Icepick scars which are deep narrow scars about 2 mm in diameter
- Boxcar scars which are wider with sharp vertical edges
- Rolling scars which are about 4-5 mm wide and caused by the dermis being attached to the subcutaneous tissue underneath, giving the skin a rolling appearance
2. Hypertrophic and keloidal scars
Due to increased collagen synthesis within the injured skin areas, with restricted turnover due to low collagenase activity. These are pink elevated scars limited to the site of acne lesions.
The Goodman and Barron system classifies acne scarring as follows:
- macular or mildly atrophic
- moderately atrophic
- punched out or linear-troughed severe scars
- hyperplastic papular scars
Atrophic scars
In most cases, available treatments for atrophic scars include:
1. Resurfacing the skin
- Ablative (CO2 or Erbium YAG) lasers to remove superficial skin layers and encourage the growth of new epithelium, healing the wound and promoting collagen production
- or non-ablative (NdYAG or Diode) lasers to tighten the collagen fibers under the skin
- fractional photothermolysis using lasers to create microwounds in a grid pattern at a specified depth beneath the epidermis, so that healing takes place from the islands of healthy tissue between the injury locations, to even out the skin surface
2. Dermabrasion and microdermabrasion
This refers to the removal of damaged skin by physical means, to help new skin to grow over the scarred areas. While the first method removes the whole of the treated epidermis, the second removes only the superficial layer.
3. Chemical peeling
To remove the scarred superficial keratinized layer of skin and encourage regrowth. Agents used include:
- Glycolic acid
- Trichloroacetic acid (TCA) and the TCA CROSS method (Chemical Reconstruction of Skin Scars) with detailed application of 50-90% TCA to the scars
- Jessner’s solution (salicylic acid, resorcinol, and lactic acid in 95% ethanol)
- Salicylic acid
- Pyruvic acid
4. Soft tissue augmentation
In order to add height to the skin in the case of deep atrophic scars
5. Undermining the scar
6. Punch biopsy excision
This is to remove the atrophic area is often combined with soft tissue augmentation
Hypertrophic scars
Hypertrophic scars are treated with:
- Silicone gel application to improve skin thickness by at least 40-50%
- Injection of corticosteroids into the lesion to inhibit collagen synthesis and promote collagenolysis, reducing the bulk of the scar
- Cryotherapy with liquid nitrogen to reduce the size of these scars by slowing blood flow, is used alone or preceding intralesional steroid injections
- Pulsed dye laser
- Surgery such as W-plasty or autologous tissue transplants
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2958495/
- http://www.aafp.org/afp/2004/0501/p2123.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4570086/
Further Reading
- All Acne Content
- Acne
- Acne Causes
- Acne Treatments
- Acne and Women
Last Updated: Feb 26, 2019

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Source: Read Full Article
