Vaginitis Treatment
Successful vaginitis treatment hinges on the proper diagnosis being made initially, in order for the most appropriate treatment to be implemented. This is because the treatments vary considerably according to the cause of the inflammation in the vaginal area.
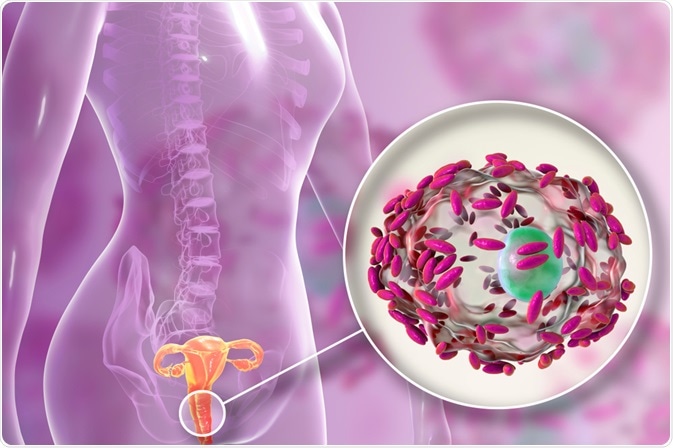 Image Credit: Kateryna Kon / Shutterstock.com
Image Credit: Kateryna Kon / Shutterstock.com
Differential diagnosis
Differential diagnosis is usually made by conducting a history of the symptoms, particularly in relation to the characteristics of the vaginal discharge.
- A candida infection is characterized by a thick, white discharge with no distinctive odor.
- A bacterial infection can lead to various types of discharge, from milky white to frothy green, depending on the causative bacteria. It may have a strong odor, often described as similar to fish.
- A chemical irritant is likely to cause redness and itchiness in the area but is not usually associated with a change in vaginal discharge.
Candida infection treatment
A candida infection is a type of fungal infection that involves the overgrowth of the normal flora of the vagina. Rather than to eradicate the candida from the area, therefore, the aim of treatment is to reset the normal candida balance, resulting in the subsiding of symptoms.
In most cases, an antifungal medication such as clotrimazole, econazole or miconazole is recommended. There are several different administration forms available, including vaginal cream and pessaries that are taken for varying lengths of time. Standard treatment length is either four or six days, with the longer treatment time recommended for those women that are prone to persistent candida infections.
Pregnant women can use antifungal pessaries to treat vaginitis caused by a candida infection. However, it is important that they insert the pessary with their fingers rather than the applicator, as this helps to reduce the risk of damage to the cervix that could affect the baby.
Bacterial infection treatment
If vaginitis is caused by the presence of bacteria in the vagina, antibiotics are the first-line choice of treatment to eradicate the bacteria and improve the symptoms. The choice of antibiotic depends on the bacteria that are present, but metronidazole is the most commonly used.
Bacteria cause sexually transmitted infections such as chlamydia, gonorrhea and trichomoniasis and patients should be advised to inform recent sexual partners of their diagnosis so that they can also seek treatment. This is because the bacteria can be passed on via sexual activity, also explaining why sexual intercourse should be avoided during treatment.
It is important that patients finish the entire course of antibiotics, even if their symptoms have subsided. This helps to prevent recurrence of infection and to ensure the bacteria are eradicated completely.
Chemical irritation treatment
If vaginitis is caused by contact with an irritant, the first step in the treatment plan should involve its removal or discontinuation of use.
Although symptoms usually resolve upon removal of the offending agent, topical corticosteroids may also offer a benefit but must be used cautiously to avoid a local sensation of burning. Other symptomatic treatments include sodium bicarbonate baths and the topical application of vegetable oil.
Prevention
Women that suffer from vaginitis on a regular basis may benefit from certain techniques to prevent future infections.
Good personal hygiene is important, although women should be aware that the vagina has a self-cleaning mechanism via the discharge it naturally produces. Many hygienic products intended for use in the pubic area are not well suited to the vagina and may upset the pH balance. Additionally, douching (flushing the vagina with water) is not recommended as it also can upset the natural balance of the vagina and cause irritation, or mask the symptoms of an infection.
Particularly in the prevention of sexually transmitted diseases that can lead to vaginitis, it is important an adequate method of protection, such as a condom, is used when having sexual intercourse. This is even more vital when an individual has multiple sexual partners.
References
- http://www.aafp.org/afp/2011/0401/p807.html
- http://www.nhs.uk/Conditions/Thrush/Pages/Treatment.aspx
- http://www.nhs.uk/Conditions/Bacterialvaginosis/Pages/Treatment.aspx
- http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/womens-health/vaginitis/#treatment
Further Reading
- All Vaginitis Content
- Vaginitis – What is Vaginitis?
- Vaginitis Causes
- Vaginitis Diagnosis
Last Updated: Jan 27, 2021

Written by
Susan Chow
Susan holds a Ph.D in cell and molecular biology from Dartmouth College in the United States and is also a certified editor in the life sciences (ELS). She worked in a diabetes research lab for many years before becoming a medical and scientific writer. Susan loves to write about all aspects of science and medicine but is particularly passionate about sharing advances in cancer therapies. Outside of work, Susan enjoys reading, spending time at the lake, and watching her sons play sports.
Source: Read Full Article
