Coronavirus: What happens when we test lots of people as cases are falling

Testing for coronavirus is increasingly recognized as essential for getting life back to normal. Free rapid testing is now being offered to the families of all pupils in England under the government’s plan to reopen schools. Similarly, every person in Germany will soon be entitled to a weekly test.
But as cases fall—thanks to lockdown and vaccine rollout—there are growing concerns about what the mass test results actually mean and whether the effect of “false positives” or “false negatives” makes them unreliable. Let’s take a look at what tests are available and how they can successfully be used to guide public health policies.
An ideal COVID test needs to be cheap, fast, easy to use and reliable. It needs to be sensitive enough to identify those infected, even if they don’t show symptoms. But it also needs to be accurate and not cause lots of false alarms, undermining its effectiveness. There is no single test that perfectly satisfies all of these conditions. Different approaches are needed to achieve this task.
The virus levels can be detected in a person even before symptoms start or if they are asymptomatic. The two main techniques used to identify a current infection are the PCR test, which detects viral RNA, and antigen tests, such as lateral flow tests (LFTs), which detect a protein that is part of the structure of the virus. There are also antibody tests, which identify people who have been infected but who aren’t currently infected or infectious.
Sensitivity and specificity
A test’s sensitivity is the way of measuring how good it is at detecting the virus or the body’s reaction to it. PCR and antibody tests are highly sensitive and can identify 98% or more of cases. However, both need specialized labs or medical assistance. In contrast, antigen tests are quick, inexpensive, and anyone can use them. However, their sensitivity is limited—ranging from a high of 90%-95% to a low of 40% when used by untrained personnel or for asymptomatic individuals.
Specificity, in turn, describes the ability of the test to determine whether a person does not have an infection. Tests typically have high specificity, as 98% or more people with no current or past infection are correctly identified. An analogy is seeking a needle in a haystack: it is not easy to find the needle (low sensitivity), but once found, it can easily be identified (high specificity).
Sensitivity and specificity affect the test result and its ability to reflect the true situation. Two cases are particularly concerning: false negatives, where an infected person is given a negative result, and false positives, where a person is incorrectly told they are infected.
False positives
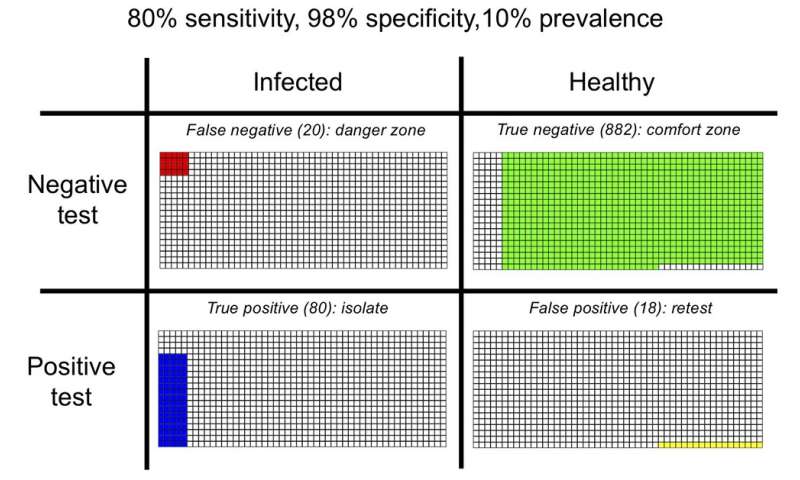
The figure below shows what could happen in a population of 1,000 people with a 10% prevalence of the virus (the proportion of currently infected people), using a test similar to the Sofia antigen test, with 80% sensitivity and 98% specificity. Out of 100 infected people, we would expect 20 to be mistakenly given the all-clear (false negatives) and 80 correctly identified (true positives). At the same time, out of 900 healthy people, 18 will be wrongly told they are infected (false positives).
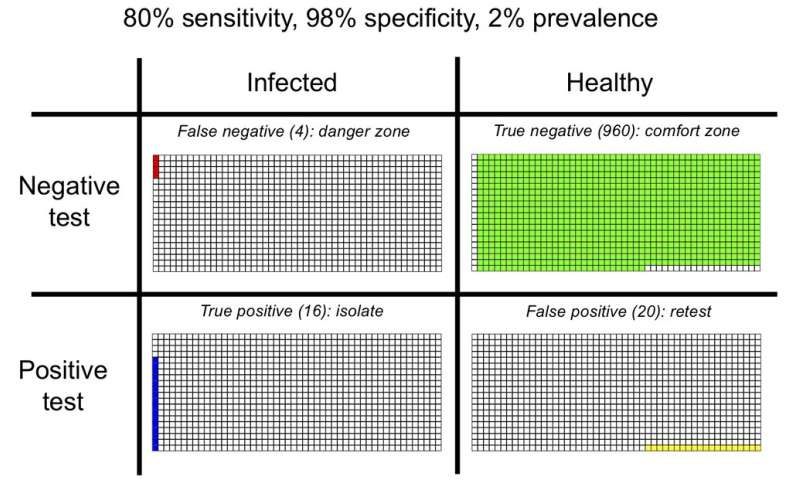
As the infection rate drops to 2%, there are only 20 infected people among 1,000, 16 (80%) of which are successfully detected. But, out of 980 healthy people, 960 (98%) are correctly identified as such, while 20 (2%) are given positive results incorrectly. The test now produces more false positives than true positives. As the epidemic is brought increasingly under control and the infection rate falls further, many more healthy than infected people might be told to self-isolate.
However, having more false than true positives is not necessarily a big problem. If a healthy person is told they have COVID in a false positive case, they will need to self-isolate—and so will their family, friends and contacts. While this might lead to a temporary hardship, there are hardly any epidemiological consequences. Besides, further accurate tests like PCR are recommended in such cases to reduce the number of false positives.
False negatives
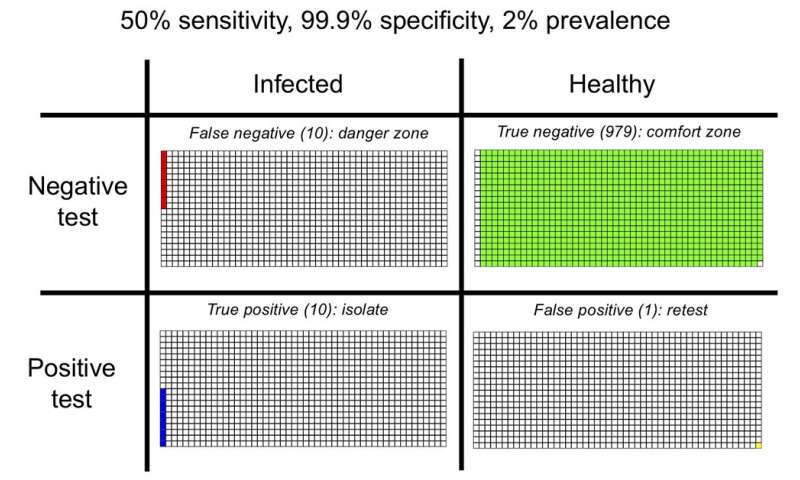
The lateral flow tests currently used in the UK are reported to be highly accurate in the virus detection with the specificity of at least 99.9%. This is reassuring as it means fewer false positives than in the example above. However, their sensitivity is potentially as low as 50%, which might create a problem with false negatives, as illustrated below.
The consequences of false negatives are potentially grave. An infected person might get a negative result and carry on with everyday life. The wrong advice could lead to further infections and, if a person is involved in a super-spreader event, could result in a large outbreak.
However, this does not mean the LFTs or similar tests are inadequate. They are cheap, fast and easily applied, so are used to quickly identify infectious but asymptomatic people. When combined with more sensitive and specific tests, they can prevent further outbreaks.
Source: Read Full Article
