Leukemia cure raises hope for more patients
Bill Ludwig and Doug Olson’s own immune cells cured them from cancer.
In 2010, the two men were battling a type of blood cancer called chronic lymphocytic leukemia that was once deemed incurable.
Both had undergone several rounds of traditional treatments, but their cancer kept coming back. Out of options, they volunteered for a clinical trial of an experimental therapy at the University of Pennsylvania that would modify their own cells to target and selectively kill cancer cells. The approach is known as CAR-T cell therapy.
More than a decade after becoming the first participants of the groundbreaking trial, Ludwig and Olson remained cancer free. An analysis of the two patients, published this month in the journal Nature, shows that the modified cells were still detectable in their bodies.
“We can now conclude that CAR-T cells can actually cure patients with leukemia,” Carl June, the immunotherapy professor at Penn who pioneered the therapy, said during a Feb. 1 news briefing.
Tens of thousands of cancer patients have since received CAR-T cell therapies, and several of these treatments have been approved by the Food and Drug Administration. CAR-T cell therapies are now given worldwide, including locally at the AHN Cancer Institute and UPMC Hillman Cancer Center. While it doesn’t represent a cure for all cancer patients, CAR-T cell therapy is particularly promising for adults with hard-to-treat blood cancers, as well as children with leukemia.
“It’s a remarkable advance in this area of treatment of cancer, and it holds the promise to be adapted to treat other forms of cancer, particularly those that are seen much more frequently,” John Lister, chief of the division of hematology and cellular therapy at the AHN Cancer Institute, said.
“It’s that sort of success that you really marvel at and want to try and duplicate and extend for all the other patients that we see,” he said.
The news of the Penn patients came the same week as President Joe Biden relaunched the Cancer Moonshot initiative with the goal of reducing the death rate from cancer by at least 50% over the next 25 years. He noted that the death rate has already fallen by about 25% in the past 20 years, in part because of new treatments like CAR-T cells and other immunotherapies.
How does car-t therapy work?
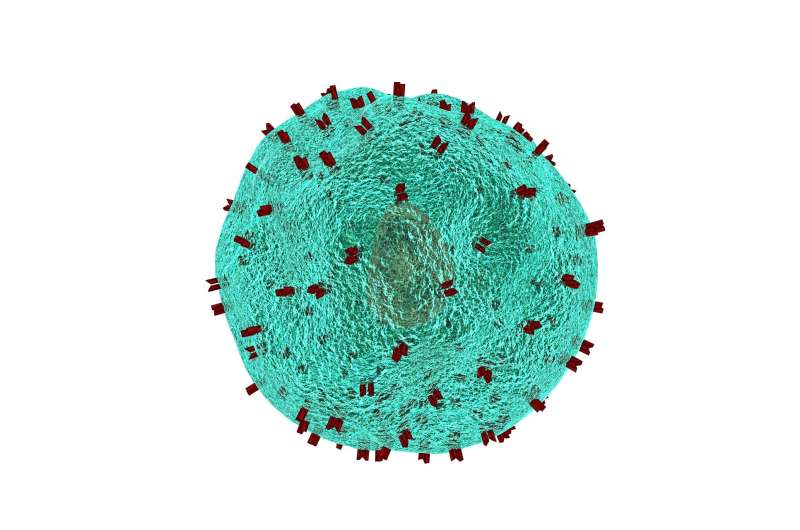
CAR-T therapy involves collecting a patient’s T cells, an important part of the immune system, by separating them from the blood. In the lab, scientists use genetic engineering to add a receptor on their surface that allows them to recognize and attach to a specific protein on cancer cells. Scientists then grow more of these cells in the lab and infuse them back into the patient.
How is CAR-T different from traditional cancer treatments?
CAR-T cells are often referred to as a “living therapy.” They’re different from traditional cancer treatments like chemotherapy, radiation and surgery because they come from a patient’s own cells. The treatment is tailored to each individual patient.
“It uses the patient’s own immune system,” said Alison Sehgal, a hematologist and medical oncologist at UPMC Hillman Cancer Center. “It’s able to adjust the patient’s immune system to find the cancer cells and kill them.”
Another major difference is that chemotherapy and radiation kill healthy cells along with cancerous cells, often causing hair loss, nausea and extreme fatigue. CAR-T doesn’t have the same sort of toxicity as traditional cancer treatments.
“It is not without side effects, but the side effects are decidedly different from what you experience with conventional therapy,” Lister said.
Who’s eligible to get CAR-T cell therapy?
CAR-T cell therapies are only approved to treat certain types of leukemias and lymphomas in children and adults. The CAR-T cells are engineered to target a protein called CD19, which is found in abundance in blood cancers.
“It’s a limited set of diseases that have this particular protein on their surface,” Lister said, “Right now, it wouldn’t do anything for breast cancer, colon cancer, lung cancer, or stomach cancer, for instance.”
To be a candidate for CAR-T cell therapy, patients with these cancers need to have failed two attempts of traditional cancer treatment first—in other words, their cancer didn’t respond to treatment or came back after treatment.
“We believe that it will shortly be available to patients who don’t respond to a first-line therapy in these particular diseases,” Lister said.
How effective is it?
The success rate for CAR-T cell therapy is around 30% to 40% for lasting remission.
“Whether or not that translates to a cure I think is what’s making people so excited about this current paper,” Sehgal said. “Could it be that people who have two- or three-year remissions will eventually be considered cured? That’s a question we haven’t been able to answer.”
What are the side effects?
CAR-T cell therapy can sometimes cause serious or even life-threatening side effects. One is an inflammatory response called cytokine release syndrome, which causes a fever and flu-like symptoms. The other is called immune effector cell associated neurological toxicity, a neuropsychiatric syndrome that can manifest as confusion, difficulty speaking and extreme tiredness.
Doctors have standardized approaches to treat both of these conditions, and most patients who get these side effects recover quickly. CAR-T cell therapies don’t cause hair loss like traditional cancer therapies do.
What are the approved CAR-T cell therapies?
The FDA has approved five CAR-T cell therapies: Kymriah, Yescarta, Tecartus, Breyanzi and Abecma.
Will CAR-T be available for more cancers?
Scientists are trying to develop CAR-T and other cell therapies for more types of cancer. But getting them to work in solid tumors—including breast, colon and pancreatic cancer—has been challenging. Studies have found that CAR-T cells aren’t able to effectively penetrate solid tumors, get inside and stick around long enough to kill cancer cells.
Source: Read Full Article
