Predicting whether bowel cancers will respond to immunotherapy
Scientists from the Francis Crick Institute and King’s College London have studied colorectal cancer and found that levels of specific immune cells are the best predictors of whether immunotherapy will be effective in individual patients.
Colorectal cancer, also known as bowel cancer, is cancer of the colon or rectum and typically affects older adults but can occur at any age. In addition to treatments like surgery or chemotherapy, some patients might also receive immunotherapy to help harness the body’s ability to recognise and fight the cancer.
While some patients respond well to a type of immunotherapy called immune checkpoint blockade, which stop proteins on the surface of cancer cells from disrupting immune cell activity, others do not. Understanding why this treatment works in some cases but not others would help doctors identify the most effective way to treat an individual patient as well as help scientists uncover new ways to make this treatment effective for even more people.
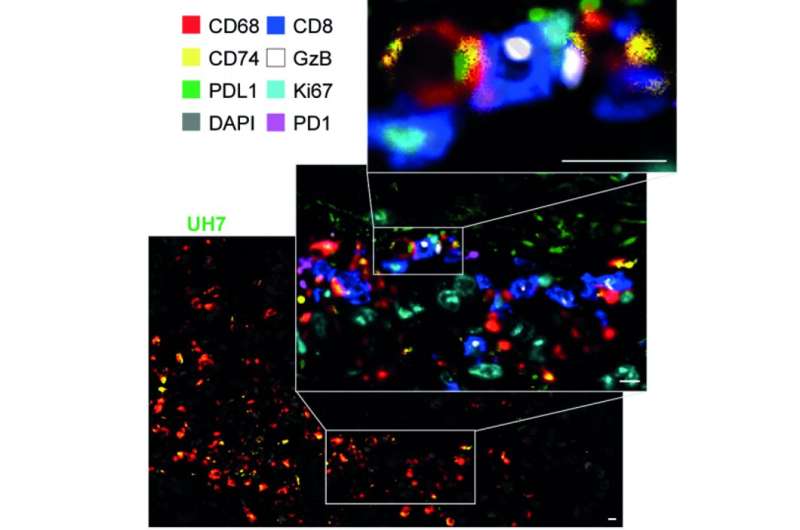
In their paper, published in Gastroenterology, the scientists took over 700 samples of cancer tissue and surrounding non-cancer cells from 29 patients treated with immune checkpoint blockade as part of international clinical trials. By sequencing the tumour DNA and using mass cytometry to identify the types and levels of immune cells in the samples, the team obtained a very detailed molecular and cellular 3D map of each tumour.
Francesca Ciccarelli, senior author of the study, group leader of the Cancer Systems Biology Laboratory at the Crick and Professor of Cancer Genomics at King’s College London, says: “We combined the expertise of clinicians, immunologists, computational biologists and cancer geneticists to study the response of patients with colorectal cancer to immune checkpoint inhibitors from different angles. This allowed us to have a complete picture of all actors involved. Our study illustrates how cutting-edge technology and interdisciplinary research are essential to understand the mechanisms of action of novel treatments, such as cancer immunotherapy.”
The researchers found that there were a number of factors which influenced whether the immunotherapy was likely to be effective.
The key predictor was the levels of a particular group of immune cells, called PDL1+ antigen-presenting macrophages. These macrophages interact with other immune cells, PD1+ CD8 T cells, preventing them from attacking the cancer cells. The researchers suggest that this interaction is disrupted when immune checkpoint blockade drugs are administered, thus releasing PD1+ CD8 T cells that can kill the cancer.
They also found other signs that could help predict whether the treatment would be effective. Patients who were more likely to benefit from the immunotherapy had cancer cells with many of the same mutations. Mutations spread across the tumour help the immune system to recognise and kill several cancer cells at the same time.
Source: Read Full Article
