Researchers improve the standard method for assessing cardiovascular disease risk
Taking into account two common kidney disease tests may greatly enhance doctors’ abilities to estimate patients’ cardiovascular disease risks, enabling millions of patients to have better preventive cardiovascular care, according to a large international study co-led by researchers at the Johns Hopkins Bloomberg School of Public Health.
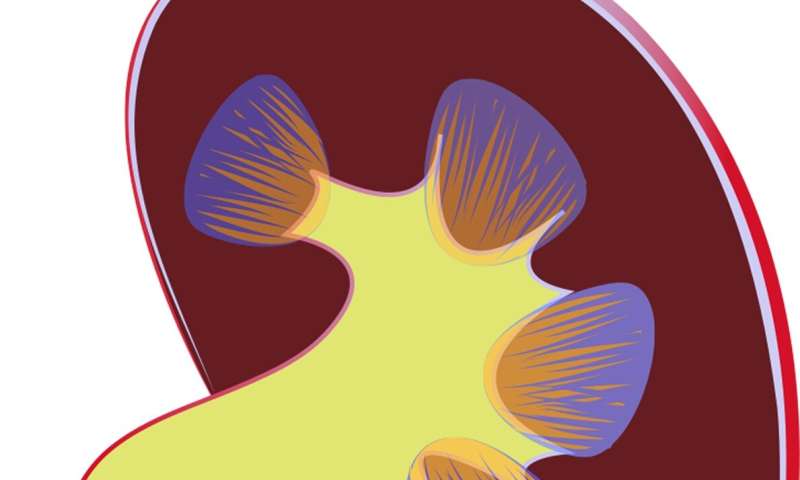
The researchers used data from more than nine million individuals around the world to develop and validate a risk-scoring calculation that adds blood and urine measures of kidney disease to the current standard method in the United States for assessing cardiovascular disease risk. The two measures—estimated glomerular filtration rate and urine albumin—are commonly used to reveal chronic kidney disease. CKD, as it’s called, has long been considered a risk factor for cardiovascular disease, although until now CKD-related measures have not been included in standard algorithms for quantifying cardiovascular disease risk.
The researchers showed that the use of their “CKD patch”—a computer-program update—can result in large increases in cardiovascular disease-risk estimates among patients with severe CKD.
The investigators also developed a similar patch to enhance the standard risk-assessment tool used in Europe.
The study appears October 14 in EClinicalMedicine, a new online open-access journal published by The Lancet.
“Adding these two measures of kidney disease, which are frequently available from blood and urine tests at checkups, allows potentially big improvements in the accuracy of a patient’s risk estimates—improvements that should in turn enable doctors to optimize patient care,” says study co-first author Kunihiro Matsushita, MD, an associate professor in the Bloomberg School’s Department of Epidemiology.
“This is a big deal—an estimated ten percent of the United States adult population has kidney disease and potentially would benefit from improved care if this new tool is adopted,” says co-last author Josef Coresh, MD, George W. Comstock Professor in the Department of Epidemiology at the Bloomberg School.
The other co-first author was Simerjot Jassal, MD, of the University of California, San Diego, and the other co-last author was Elke Schaeffner, MD, of Charité University Hospital Berlin. Shoshana Ballew, Ph.D., assistant scientist in the Bloomberg School’s Department of Epidemiology, helped coordinate the data-gathering. In all, the study included more than 50 researchers.
The reduction of kidney function in CKD can lead to higher blood pressure as well as hormonal and other chemical imbalances, and these in turn promote the narrowing of arteries that supply the heart muscle—conditions known as atherosclerosis and arteriolosclerosis. The American Heart Association and the American College of Cardiology, in their guidelines for physicians, already list CKD as a “risk enhancer” for atherosclerotic cardiovascular disease, but without a specific tool that quantifies the added risk as part of the standard risk calculator.
Since 2009, Coresh, Matsushita, and colleagues have been assembling a large, international database of CKD patients and healthy adults, under a collaboration known as the CKD Prognosis Consortium. For the new study, they analyzed a portion of this database, covering 4.1 million adults around the world, to develop algorithms that estimate cardiovascular disease risk using standard measures plus the two kidney-disease measures. They then validated the accuracy of their algorithms using further samples covering 4.9 million adults.
The two kidney disease measures, estimated glomerular filtration rate and urine albumin, respectively, indicate the kidneys’ blood-filtering efficiency and the level of an essential protein called albumin that the kidneys normally would filter out of the urine.
The researchers incorporated these measures in a ‘CKD patch’ to the standard cardiovascular disease-risk estimation algorithm developed by the American Heart Association and the American College of Cardiology. They found that for adults who had results on these kidney- disease tests indicating CKD, the addition of these measures via the CKD patch significantly improved the estimated 10-year risks of atherosclerotic cardiovascular disease.
For example, for patients with ‘very high-risk’ CKD, the estimated 10-year chances of developing atherosclerotic cardiovascular disease were a median of 1.55 times higher than estimates without the CKD patch, while the figures were a median of 1.24 times higher for “high-risk” CKD patients.
The researchers’ CKD patch for the standard European 10-year cardiovascular disease mortality risk estimator also boosted estimated risks, by a median of 2.64 times in very high-risk CKD patients, and 1.86 times in high-risk CKD patients.
“These results suggest that doctors have tended to underestimate cardiovascular disease risks in kidney disease patients,” Matsushita says.
The researchers hope that their CKD patches will be adopted widely, enabling more accurate assessments of cardiovascular disease and related mortality risks—which in turn should result in better preventive care including the use of statins and other interventions to ward off cardiovascular disease.
Source: Read Full Article
