You’ve had a COVID ‘breakthrough infection’—can you spread it to others?
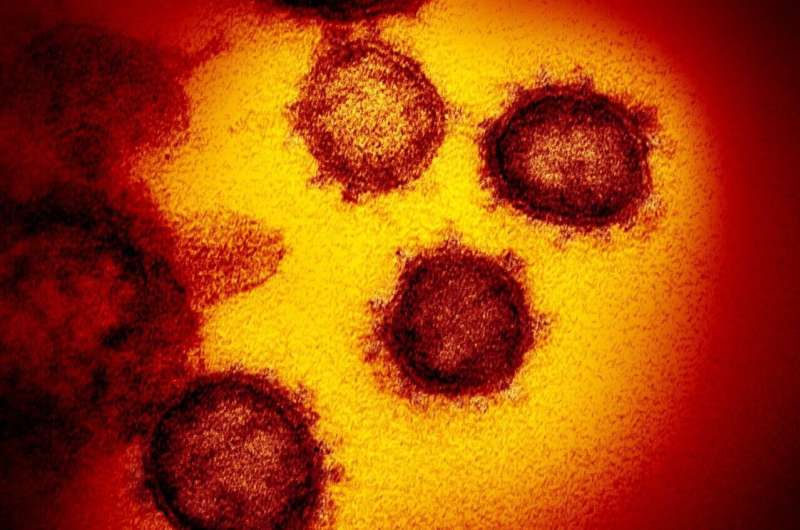
COVID-19 breakthrough infections—where a fully vaccinated person becomes infected with the coronavirus—are occurring across the globe, due, in large part, to the highly contagious Delta variant. Here in the United States, many Americans are concerned for their unvaccinated loved ones, including children and those who are immuno-compromised—and given this news, for themselves as well.
Many of us believed that the COVID-19 vaccines offered complete protection from infection, not just from severe disease and death. And though these breakthrough cases are relatively rare, they are a reminder that the pandemic is far from over.
Apart from getting sick, there is also worry that with the Delta variant, a fully vaccinated person who becomes infected may spread the coronavirus to others. According to recent reports from the Centers for Disease Control and Prevention (CDC), this can happen—a finding that may be a game-changer, affecting decisions on how to safely go back to school; return to the office; attend concerts or theater and sporting events; and even whether it’s safe to date.
“The CDC data comes at a critical time, when cases—mostly due to the Delta variant—are on the rise in the U.S. Areas with low vaccination coverage are being hit especially hard with the highest daily case rates in months,” says Yale Medicine infectious diseases expert Jaimie Meyer, MD, MS. “Even though many people were ready to throw away their masks and get back to ‘normal’ life this summer, the latest spikes show us that the pandemic persists. We have to use the CDC data to reassess our understanding of our personal and community risk.”
Breakthrough cases and Delta: Background
Until recently, scientists were unsure whether fully vaccinated people who became infected with COVID-19 could transmit it to others. But the CDC report released in late July made it clear that some vaccinated people can get Delta in a breakthrough infection—and may be contagious.
The CDC added that breakthrough infections “occur in only a small proportion of vaccinated people and of the breakthrough infections, transmission by the vaccinated appears to only be a small part of overall spread of the virus.” But the CDC says it does not yet have data on the likelihood of asymptomatic spread among vaccinated people.
So, where does that leave us?
What we do know, says Dr. Meyer, is that there is less circulating virus in the community as a result of vaccination. “When we look at vaccinations compared to cases on a population level—[view the CDC COVID Data Tracker]—we see that as the number of people vaccinated rises, the number of cases decreases,” she says. “This is likely due to the fact that people who are vaccinated are not becoming infected as often, but also that they are not ‘forward-transmitting’ the virus as often.”
But more research is needed. The CDC says that “studies are underway to understand the level and duration of transmissibility from Delta vaccine breakthrough infections.”
Trials focused on infection, not on transmission
How can it be that after conducting clinical trials that involved tens of thousands of people, there was still uncertainty about whether the three authorized COVID-19 vaccines—from Pfizer-BioNTech, Moderna, and Johnson & Johnson—could prevent or reduce transmission?
In large part, it’s because the clinical trials for these vaccines were primarily focused on determining whether the vaccines protected against symptomatic COVID-19 infection. And though the trials showed that the vaccines are very effective in preventing severe disease, hospitalization, and death, none were found to be 100% protective against infection, meaning that some trial participants had mild or asymptomatic COVID-19 cases, even after vaccination.
With the initial coronavirus strain, or even with the Alpha variant, the post-vaccine immune response is usually fast and potent enough that it clears out the infection quickly—before the virus can spread far in the body or serious symptoms have a chance to develop. But because infection could technically occur, transmission was still considered a possibility—albeit a remote one.
But those trials were conducted prior to the emergence of what the CDC refers to as “variants of concern”—mutated versions of SARS-CoV-2, the virus that causes COVID-19. Evidence shows that these variants may be more transmissible and may cause more severe disease than the original strain. What’s more, vaccines may be less effective against some of them, including Delta, which is now the dominant variant here in the U.S.
“The Delta variant is showing every day its willingness to outsmart us,” said CDC director Rochelle Walensky, MD, MPH, at a recent news briefing.
What’s required for a vaccine to be 100% effective at preventing infection
In order to entirely prevent infection, vaccines would need to induce what’s called “sterilizing immunity,” a type of immunity that prevents a pathogen—in this case the coronavirus—from infecting any cells. If the virus cannot infect cells, then the host (in this case, a person) cannot transmit it to others.
In a best-case scenario, all vaccines would provide sterilizing immunity, meaning they would protect against disease and prevent transmission. But in practice, most vaccines don’t do this. The influenza, rotavirus, and pertussis vaccines, among others, can prevent serious illness from developing, but they don’t reach the level of sterilizing immunity.
The same is true for the three authorized COVID-19. But studies of the real-world effectiveness of the Pfizer-BioNTech and Moderna vaccines suggest that they can substantially reduce the risk of infection. (Researchers are still gathering real-world info about how well the Johnson & Johnson vaccine protects against infection.)
And reducing infection is tied to reducing transmission. “If you’re not infected, you can’t transmit,” says Dr. Meyer. “Vaccines prevent infection; therefore, vaccines also prevent onward transmission.”
But with reports of breakthrough cases, the worry about transmissibility remains top-of-mind for many, even if—or perhaps because—there is a lack of data on all aspects of the issue. “What we don’t have—to my knowledge—is a clear epidemiologic study that maps out how many new COVID cases are directly traced back to someone who was infected after vaccination,” says Dr. Meyer.
Why don’t we have data on breakthrough cases?
Up until May 1, 2021, the CDC recorded all breakthrough cases, whether mild, moderate, or severe. But starting on May 1, they began recording only breakthrough cases that resulted in hospitalization or death. The CDC explains that they made this change to “help maximize the quality of data collected on cases of greatest clinical and public health importance.”
But this means that in the U.S. we do not know how often breakthrough cases occur or which variants are causing breakthroughs (though given that over 83% of COVID-19 cases in the U.S. are from the Delta variant, it is probable that many of the breakthrough cases, at least recently, are from Delta).
So, should you worry that a fully vaccinated person who may have an asymptomatic breakthrough case can unknowingly transmit the virus to someone who is unvaccinated?
I would say it’s not likely, but we don’t yet know with certainty, says Dr. Meyer. “Theoretically, it may be true that people are being infected by their asymptomatic vaccinated contacts, but we’re just not seeing that clinically,” she says. “And the verdict is out on this in terms of the epidemiologic data.”
Viral load and transmission
There is also another consideration—the role viral load may play in transmission. A study published in February 2021 in The Lancet Infectious Diseases found that the viral load—the amount of virus in a person’s body (in this case, in the nose and throat)—is a critical factor in the transmission of SARS-CoV-2.
Specifically, the study concluded that those with higher viral loads are more likely to transmit the virus to others. In March, another study from Israel found that the Pfizer-BioNTech vaccine, even after just a single dose, significantly reduced viral load—which suggests that it may also lower the risk of transmission. But it did not evaluate whether vaccinated people could transmit the virus, even if their viral loads were reduced. Nor did it take into account the Delta variant.
A recent study, which has not yet been peer-reviewed, demonstrated that people infected by the Delta variant had viral loads roughly 1000 times higher than those infected by the initial strain of the virus.
“The higher viral loads may play a role in increasing the risk of transmission, because each droplet can be packed with more virus,” says Dr. Meyer.
But the extent to which it does so in unvaccinated and vaccinated people is still unclear.
Other features of the Delta variant may factor into its increased transmissibility. For instance, the same study also found that those infected with this variant may become infectious—or capable of spreading the virus to others—sooner after infection than is the case for other coronavirus variants.
More research is needed
The good news is that studies are underway that directly assess transmission. Several universities in the U.S., for instance, are participating in the PreventCOVIDU study to assess whether the Moderna COVID-19 vaccine prevents transmission of SARS-CoV-2. This study will evaluate the vaccine’s ability to prevent infection, reduce viral load, and prevent transmission. Results of the study should be published later this year. Other similar studies are underway.
What can you do to stay safe?
In light of the rapid rise in COVID-19 cases, largely driven by the Delta variant, in late July, the CDC updated its COVID-19 prevention guidance. The CDC is now recommending that everyone, including the fully vaccinated, wear a mask in indoor public spaces in areas where COVID-19 transmission is substantial or high. (The CDC map provides regular updates for anyone who wants to check virus activity in their state or county. It breaks it down into four categories: low, moderate, substantial, and high.)
The new recommendations emphasize that certain populations should continue masking, for instance those who have or live with someone who has a suppressed immune system or an underlying medical condition that puts them at risk for severe disease.
The agency has also urged universal masking for teachers, staff, students, and visitors in K-12 schools, regardless of their vaccination status and the intensity of community transmission in their area.
Another substantial change to the CDC guidelines is the recommendation that fully vaccinated people who have been exposed to someone who has COVID-19 get tested. These people should also wear a mask when indoors in public areas for two weeks after exposure or until test results are negative.
“Importantly,” says Dr. Meyer, “they’re not recommending quarantine after exposure if you’re fully vaccinated—just to wear a mask and get tested. And that’s because we think post-vaccination infections are so rare.”
But if fully vaccinated people test positive for COVID-19, the CDC recommends they isolate for 10 days.
Still, because we don’t yet know anything definitive, many believe that a layered mitigation strategy (that includes fully vaccinated people wearing masks and maintaining social distance wherever possible) might be the best way to minimize the chances that they will transmit the virus to others.
Source: Read Full Article
