Risk Factors of Osteoporosis
Osteoporosis is a significant public health concern that can adversely impair health-related quality of life. Approximately 10 million adults in America have the condition, with at least two million reported causes of new osteoporotic-related fractures occurring per year.
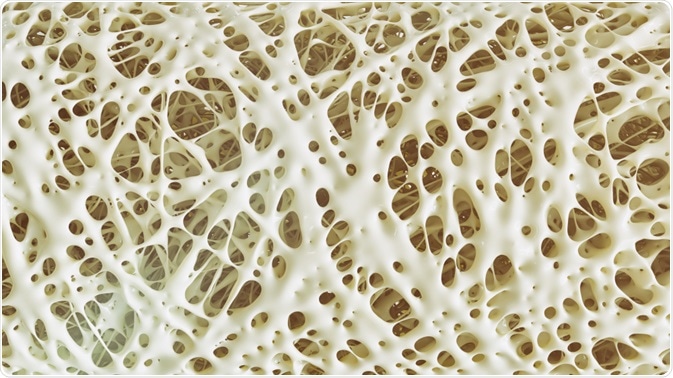
Image Credit: Crevis/Shutterstock.com
What is Osteoporosis?
Osteoporosis is a progressive skeletal disease characterized by a loss in bone mineral density (BMD) resulting in fragile, weakened bones that are more prone to break than those without the condition.
Most individuals only receive a diagnosis following a physical impact on the body or fall, which results in fractures. Such fractures commonly occur in the hips, wrists, or vertebrae. In some instances, sneezing or coughing can result in broken ribs or the partial collapse of a vertebra.
Risk Factors of Osteoporosis
Several risk factors have been associated with the onset of osteoporosis, including inflammatory bowel diseases, eating disorders, and hormonal factors.
Inflammatory Bowel Diseases
Research has found that those with Inflammatory bowel diseases, including Crohn’s disease, are more likely to have lower levels of BMD. A team of researchers from the University Hospital Heidelberg, German conducted a retrospective longitudinal study to investigate factors associated with BMD in a sample of patients with Crohn’s Disease.
Those with Crohn’s were significantly more likely to have lower bone mineral density, and therefore, a higher risk of osteoporosis, if they had undergone bowel resections, had a low body mass index (BMI) score, and were male. However, in the longitudinal course, lower levels of BMD were associated with being female, and a history of steroid and immunomodulator use.
Based on these findings, the authors argued that male patients with Crohn’s, patients with a low BMI, and a history of bowel resections should be assessed for low BMD. If done in a timely fashion, it can enable such patients to increase their bone mineral density using anti-osteoporotic therapy and prevent the onset of osteoporosis.
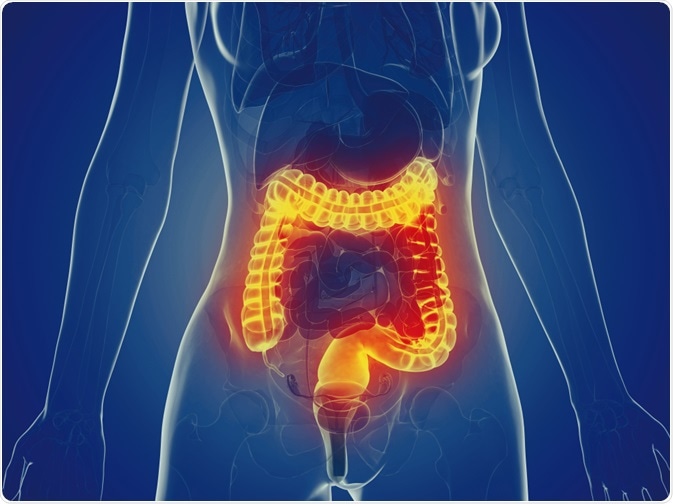
Image Credit: SciePro/Shutterstock.com
Eating Disorders
Osteoporosis is a common and adverse complication of eating disorders characterized by dramatic weight loss or low BMI. Young males and females with anorexia nervosa (AN) rapidly develop a decline in BMD following the onset of the psychiatric condition.
Unlike some of the other complications associated with AN (which can often be reversed following nutritional rehabilitation and weight restoration) practitioners find low BMD may be irreversible for such patients. These can result in a life-long increase risk of fractures.
Low BMD in those with anorexia is caused by a variety of factors, including low estrogen and testosterone levels, reduced levels of insulin-like growth factor, and increased cortisol levels.
Hormonal Factors
Hormonal factors are associated with an increased risk of developing osteoporosis in women compared to men. Estrogen is vital for healthy bones and can influence overall levels of bone density. After going through the menopause, levels of estrogen decrease, directly affecting bone mineral density.
Women are particularly most at risk if they have gone through the menopause before 45 years of age, had a hysterectomy including the removal of the ovaries before the age of 45, or if they have had no periods for more than six months due to excessive dieting or exercise.
Less is known about the contributing factors of osteoporosis in men. However, some suggest a link between the male sex hormone and BMD. Despite, men continuing to produce testosterone as they age, lower levels of the male hormone have been associated with an increased risk of osteoporosis. A low level of testosterone is linked to alcohol misuse and the consumption of specific medication, including steroids.
How to Prevent Osteoporosis
Several recommendations have been suggested for those most a risk of developing osteoporosis to maintain healthy bones. Regular exercise is crucial to maintain both cardiovascular and bone health. It is recommended that adults aged up to 64 years old should complete a minimum of 2 hours and 30 minutes of intermediate-intensity aerobic exercise, for example, hiking or cycling.
Additionally, activities that strengthen the major muscle groups should be completed two days per week alongside resistance and weight-bearing training to increase bone density and reduce the likelihood of developing osteoporosis.
Diet also plays a role in bone health and can help boost density in those most at risk of developing bone conditions. Vitamin D and calcium are both equally essential for maintaining strong bones, as vitamin D assists the body in being able to absorb calcium.
Adults are recommended to consume 10mg of vitamin D and 700mg of calcium per day, and where possible from getting a healthy, balanced diet, including foods such as yogurt, egg yolks, and salmon. Vitamin D supplements can also be used alongside healthy eating as getting sufficient amounts of the vitamin from food alone can be difficult.
References and Further Reading
- NHS (2019). Osteoporosis: Overview. https://www.nhs.uk/conditions/osteoporosis/
- Hoffmann, P., Krisam, J., Kasperk, C., & Gauss, A. (2019). Prevalence, Risk Factors, and Course of Osteoporosis in Patients with Crohn’s Disease at a Tertiary Referral Center. Journal of Clinical Medicine, 8(12), 2178. Doi: 10.3390/jcm8122178
- Sattari, M., Cauley, J. A., Garvan, C., Johnson, K. C., LaMonte, M. J., Li, W., … & Wactawski-Wende, J. (2017). Osteoporosis in the women's health initiative: another treatment gap?. The American journal of medicine, 130(8), 937-948. Doi: 10.1016/j.amjmed.2017.02.042
- Fazeli, P. K. (2019). Low Bone Mineral Density in Anorexia Nervosa: Treatments and Challenges. Clinical Reviews in Bone and Mineral Metabolism, 17(2), 65-76. Doi: 10.1007/s12018-019-09260-4
Further Reading
- All Osteoporosis Content
- Bone Disease
- What is Osteoporosis?
- Osteoporosis Symptoms
- Osteoporosis in Men
Last Updated: Sep 2, 2020
Source: Read Full Article
