Associations between mucosal gene expression and microbiome composition in three gastrointestinal disorders
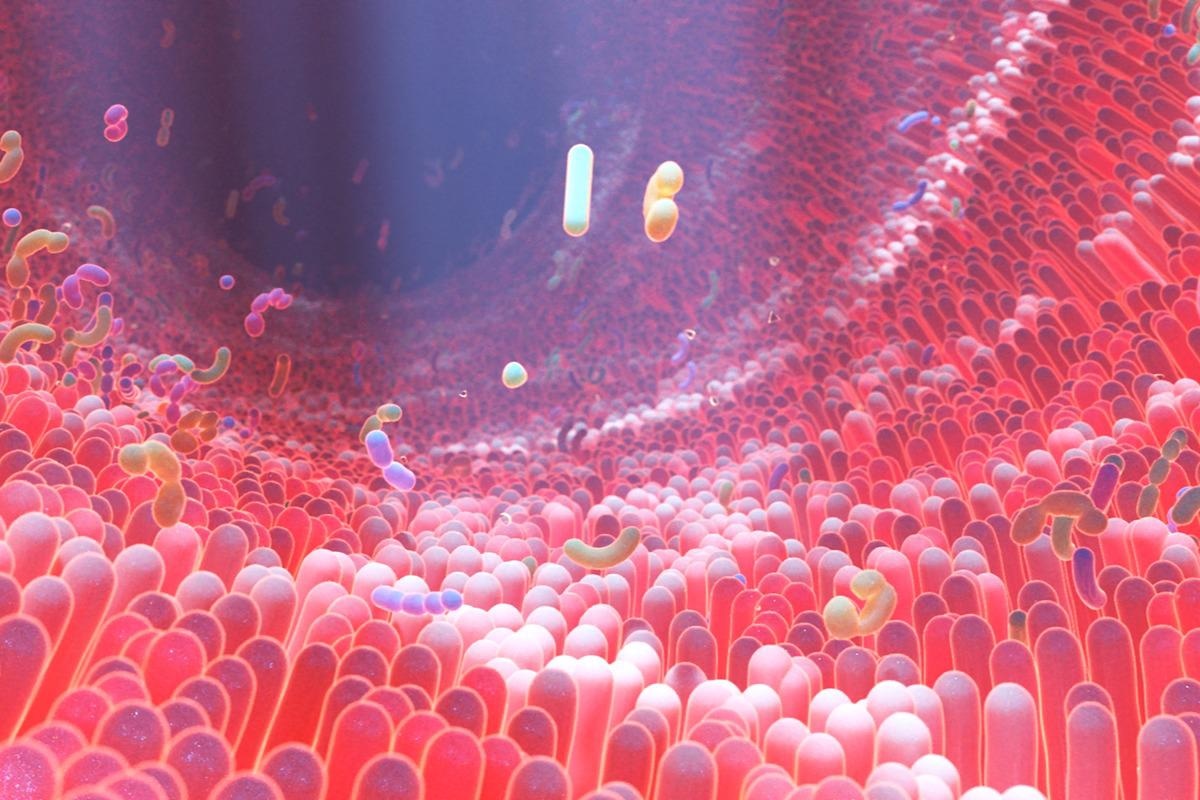
A new study authored by Sambhawa Priya and other researchers offers a detailed look at the interactions between the gut microbiome of humans in health and disease. Many chronic conditions are linked to a range of alterations in the composition of gut microflora, as well as to changes in the regulation of host genes and signaling pathways.
In this study, published as an open-access article in the journal Nature Microbiology, the authors trace the interconnections between the expression of the host genes and the gut microbiome in gastrointestinal diseases like inflammatory bowel disease (IBD) and irritable bowel syndrome (IBS).
Introduction
Many earlier studies in animal models showed the extent to which host gene expression is modulated by the gut flora, indicating the rich and deep interdependent relationship between animal physiology and gut microbes. Epigenetic changes can alter the immunological and metabolic processes in animals. Thus, understanding how these connect with and act on each other could help reveal how these diseases occur and are reinforced.
Research on colorectal cancer has shown that genes related to the expression of chemokines such as CXCL6 and DUOX2 are correlated to the enrichment of certain pathogenic gut microbes and the elevated expression of host genes that are involved in gut inflammation and tumor formation. Similar interactions have been uncovered in IBS.
However, these studies focused only on differentially expressed genes (DEGs), immune genes, or certain microbes or microbial clusters. They looked for only certain types of correlations for the most part and examined associations with one disease at a time.
“Hence, common and unique patterns of host–microbiome associations across multiple disease states remain poorly characterized.”
The current study aimed to fully delineate the correlations between the expression of mucosal genes and the gut microbiome profile in three conditions: CRC, IBS, and IBD. Using machine learning, they integrated findings from several ‘omics, to obtain true and meaningful associations between these variables in each condition.
What did the study show?
Earlier studies found both Peptostreptococcaceae and Streptococcus species to be enriched in all three conditions, while butyrate-producing bacteria were lost in CRC and IBD. However, in contrast, host genes are distinctive in their changes in each disease. IBS showed a pattern of antibacterial gene expression, with a breakdown of the purine salvage pathways. IBD is associated with the dysregulation of proinflammatory pathways, and CRC is marked by the activation of Notch and WNT pathways that signal oncogenic changes.
In this study, the researchers used two sets of samples, microbiome and host gut microbiome samples. This showed correlations between each pair in only one of three methods, indicating a selective association between some genes and some microbes. This was overcome using the machine learning approach they developed.
They found that specific gut microbes are associated with common pathways irrespective of the disease (IBS, IBD, or CRC). Other specific pathways were also implicated, where each disease showed a different pattern of correlation between gut microbes and gene expression.
The scientists chose to focus on the five most significant pathways among these.
Three shared pathways were identified, common to all three, that regulate gut inflammation, the gut epithelial barrier, and barrier repair. These include oxidative phosphorylation. Others were found to overlap pairs from these three conditions. Over a hundred pathways were also identified specific to each disease, of which over half were linked to CRC and a quarter each to each of the other two conditions. IBD-specific pathways included those associated with integrins, while those specific to IBD included immunologic pathways.
The scientists also examined the RAC1 pathway, which regulates both mucosal repair and immune response in the gut. While some shared host genes were observed across the three conditions, they were associated with different microbial groups in each disease. In IBD, for instance, it was correlated with Granulicatella and some Clostridia, but with the oncogenic Parvimonas and Bacteroides fragilis in CRC.
Common host genes were enriched for gut epithelial immune pathways but with disease-specific microbial taxa. Some microbes commonly found in inflammatory conditions were found at higher abundance in both IBS and IBD. Conversely, the same microbes produced different effects based on their interaction with different host genes and through different pathways.
An example is Streptococcus, which is associated with genes that regulate WNT and NF-κB pathways in CRC, but regulators of the macrophage response in IBS. This suggests that “although diseases can be characterized by similar microbial perturbations, these microbes can impact disease-specific pathophysiological processes through association with different host genes in each disease.”
Further studies will be necessary to understand which direction this correlation works, of course. At the same time, different microbes or sets of microbes can modulate host genes and pathways that are common to two or more of these conditions, or one specific association may be found in one particular disease. An example of the former is the association between three different microbes in IBS, IBD, and CRC, respectively, with the same PINK1 host gene and the P13-kinase/AKT signaling pathway.
The latter case is exemplified by the Syndecan-1 pathway, a regulator of tumor growth, that is correlated with Parvimonas and Bacteroides fragilis in CRC alone. “The disease-specific pattern of host gene–microbe crosstalk suggests that gut microbes, either through direct interaction with host cells or through indirect interaction (for example, via production of specific metabolites), may regulate host gene expression differently in specific disease contexts.”
Gut disorders like these are the result of many interwoven communications between microbes and host genes, both those that are unique to the disease and those that utilize common pathways triggered by different microbes, as well as those that show the same microbial profile but different host gene patterns. These findings support the importance of multi-omics studies using genomics, proteomics, microbiology, and others to provide an integrated picture of the gut microflora and host genes in the disease process.
- Priya, S. et al. (2022) "Identification of shared and disease-specific host gene–microbiome associations across human diseases using multi-omic integration", Nature Microbiology. doi: 10.1038/s41564-022-01121-z. https://www.nature.com/articles/s41564-022-01121-z
Posted in: Medical Science News | Medical Research News | Medical Condition News | Healthcare News
Tags: Bacteria, Cancer, Chemokines, Chronic, Clostridia, Colorectal, Colorectal Cancer, Gene, Gene Expression, Genes, Genomics, Immune Response, Inflammation, Inflammatory Bowel Disease, Irritable Bowel Syndrome, Kinase, Machine Learning, Macrophage, Metabolites, Microbiology, Microbiome, Phosphorylation, Physiology, Proteomics, Purine, Research, Signaling Pathway, Syndrome, Tumor

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Source: Read Full Article
