What is Bronchiolitis Obliterans Organizing Pneumonia?
Causes
Symptoms
Epidemiology
Case reports
Diagnosis and treatment
References
Further reading
Bronchiolitis obliterans organizing pneumonia, or BOOP, is an inflammatory lung disease affecting the bronchioles and alveoli. BOOP is most commonly seen in people between 40 and 60; however, it can affect anyone of any age. Infectious and non-infectious mechanisms can both cause it. BOOP is a pathological diagnosis with clinical and radiological evidence to support it. It has been linked to rheumatoid arthritis, inflammatory myopathies, and mixed connective tissue disease, among other connective tissue diseases.
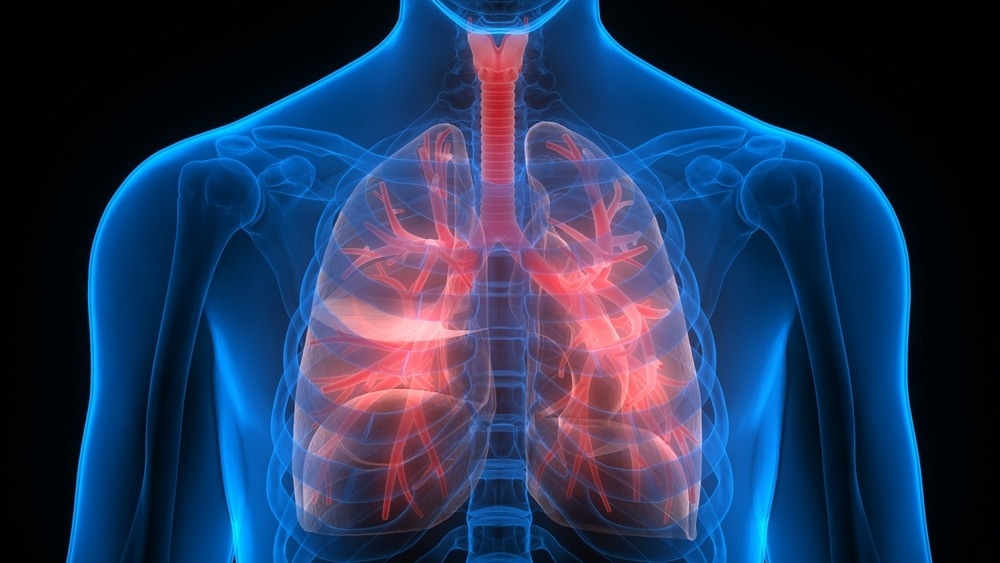
Image Credit: Magic mine/Shutterstock.com
Causes
The cause of BOOP is usually unknown, and it is referred to as idiopathic BOOP. However, both infectious and non-infectious processes can cause it. Cryptogenic organizing pneumonia is another name for idiopathic BOOP. BOOP is characterized as organized polypoid granulation tissue extending into the alveolar ducts and alveoli in the distal airways.
Rheumatologic and connective-tissue illnesses, inflammatory bowel disease, medication, inhalation of harmful gases, cocaine, and other hazardous exposure reactions, and radiation therapy to the chest are all non-infectious causes of BOOP. Because there is no fibrosing process, this inflammatory lesion is triggered by a cascade of cytokine events that varies from inflammation seen in asthma, bronchitis, and nonspecific interstitial pneumonia.
Symptoms
BOOP symptoms differ from person to person, depending on the type. Fever, cough, shortness of breath, and exhaustion are common symptoms of BOOP. Auscultation frequently produces crackles. Some people with BOOP have no symptoms, while others, like those with acute, rapidly-progressing BOOP, may have significant respiratory distress.

Image Credit: Maridav/Shutterstock.com
On chest radiographs, patchy infiltrates can be seen unilaterally or bilaterally, and CT findings can include ground-glass opacities, consolidation, air bronchograms, pleural-based triangle-shaped opacities, and the reversed halo sign. With no restriction of airflow, pulmonary function tests may reveal a drop in vital capacity and a slight decrease in diffusing capacity.
Epidemiology
BOOP affects both men and women in almost similar percentages. It usually affects people between 40 and 60, but it can afflict people of any age. BOOP is thought to be responsible for 5 to 10% of chronic infiltrative lung disease in the United States. BOOP has made headlines all around the world.
Case reports
The first instance of steroid-resistant BOOP caused by influenza was reported by Madegedara et al. in 2020. A 50-year-old man presented with a brief history of fever, pleuritic type chest discomfort, dyspnea that worsened with time, as well as hypoxemic respiratory failure.
Influenza A viral antigen was discovered in a swab of the throat. Mechanical breathing and oseltamivir therapy were started, but the patient did not respond well. BOOP was discovered on a high-resolution computed tomography (HRCT) scan of the chest. We have an infection that responded effectively to cyclophosphamide treatment.
In 2020, Ritasman et al. reported three cases of BOOP. From May to November 2018, they detailed three patients diagnosed with systemic lupus erythematosus (SLE) using the SLICC 2012 classification criteria. They were admitted to the rheumatology ward at NIMS hospital Hyderabad, India. Their diagnosis of BOOP was either confirmed by biopsy or indicated by imaging. There were three patients, one with juvenile lupus and the other two with adult lupus. Two of the patients were men, and one was a woman.
The first instance was a 32-year-old man with SLE who was admitted for a month with fever, vasculitic rash, cough, and dyspnea.
In the second case, a 14-year-old child presented with a fever, lymphadenopathy, recurring severe mouth ulcers, and a dry cough with acute onset dyspnea. SLE was present in all three individuals, with a high level of disease activity.
Third, a 34-year-old woman with constitutional symptoms, malar rash, extensive oral ulcer, and baldness arrived with sudden-onset dyspnea and productive cough after being symptomatic for three months.
They all exhibited lung manifestations of organizing pneumonia, as well as additional organ involvement. The young patient died, while the others fully recovered with steroid and immunosuppressive therapy.
Diagnosis and treatment
The most common way to diagnose BOOP is with a lung biopsy, though imaging testing and pulmonary function tests can also help. The majority of instances of BOOP react effectively to corticosteroid treatment. If a drug is to contribute to the disease, discontinuing the drug can help the patient feel better.

Image Credit: MedicalWorks/Shutterstock.com
Cyclophosphamide, erythromycin in the form of azithromycin, and Mycophenolate Mofetil have all been documented in the medical literature to be effective for patients on a case-by-case basis (CellCept). More research is needed to determine the long-term effectiveness and safety of these prospective therapy options for people with BOOP.
Individuals with BOOP who do not respond to traditional treatment choices may require lung transplantation in rare situations. Individuals with secondary BOOP may improve once the underlying issue is addressed. Symptomatic and supportive treatment is also available.
References
- Baisya, R., Devarasetti, P. K., Uppin, S. G., Narayanan, R., Rajasekhar, L., & Sreejitha, K. S. (2021). Bronchiolitis obliterans organizing pneumonia as the pulmonary manifestation of lupus: A review of three cases. Lupus, 30(2), 336–341. https://doi.org/10.1177/0961203320967439
- Dushantha Madegedara, Ishelda Nawarathne, Lihini Basnayake, S. A. Luckmy, and B Imbulpitiya. (2020). NOVEL APPROACH TO MANAGEMENT OF SECONDARY BRONCHIOLITIS OBLITERANS ORGANIZING PNEUMONIA FOLLOWING INFLUENZA A. International Journal of Research -GRANTHAALAYAH, 8(10), 292-297. https://doi.org/10.29121/granthaalayah.v8.i10.2020.2028
- Epler G. R. (2011). Bronchiolitis obliterans organizing pneumonia, 25 years: a variety of causes, but what are the treatment options? Expert review of respiratory medicine, 5(3), 353–361. https://doi.org/10.1586/ers.11.19
- Bronchiolitis obliterans organizing pneumonia. [Online] NIH-GARD. Available at: https://rarediseases.info.nih.gov/diseases/5961/bronchiolitis-obliterans-organizing-pneumonia#
- Bronchiolitis Obliterans Organizing Pneumonia. [Online] National Organization for rare disorders. Available at: https://rarediseases.org/rare-diseases/bronchiolitis-obliterans-organizing-pneumonia/
Further Reading
- All Pneumonia Content
- Viral vs Bacterial Pneumonia
- Pneumonia Symptoms and Risk Factors
- Pneumonia Classification
- Pneumonia Cause
More…
Last Updated: May 2, 2023
Source: Read Full Article
